Antimicrobial Agents in the Food Chain – Use and Misuse
Quality, safety and preservation of food products are universal concerns. Food producers and handlers use antimicrobial agents to prevent spoilage of food as well as to prevent food-borne illnesses. Antimicrobial agents such as antibiotics and anti-fungal drugs extend the shelf life of food products. Now, there are two sides to the use of such drugs. On the one hand, their increasing use may have helped in addressing food-borne illnesses and given us food products with longer shelf life, but on the other hand this has triggered a situation where constant exposure has made human beings resistant to these drugs. This article explains the implications of such antimicrobial resistance (AMR) and why it is a major concern.
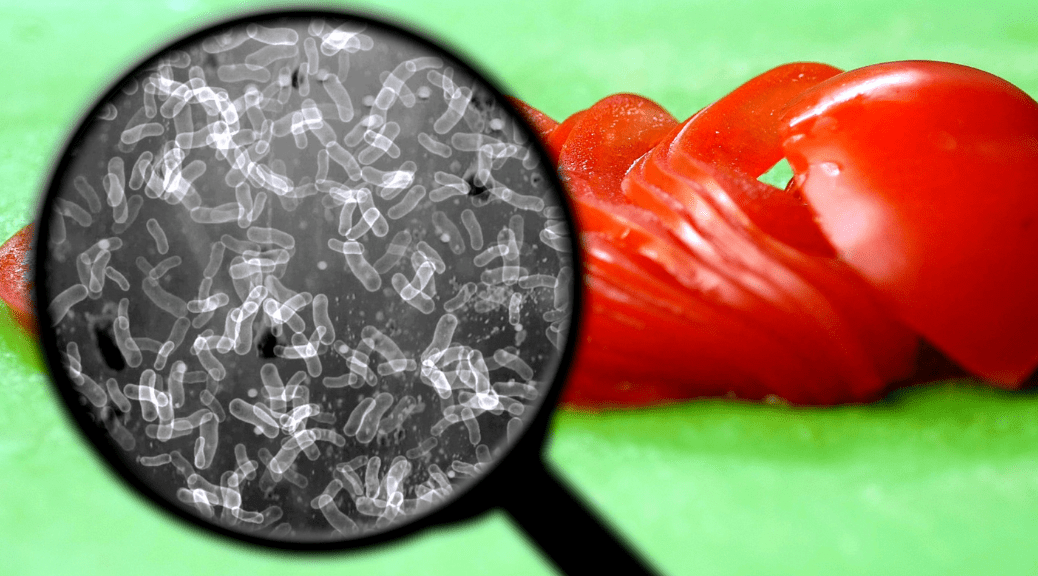
For one, constant exposure to antimicrobial agents damages the microbes that are helpful and in fact are needed for certain biological processes to happen in human beings (lactobacillus, for example, lives in the intestine and helps digest food). Antimicrobial resistance (AMR) is a more severe result of such exposure. Repeated, improper use of antibiotics—in both humans and animals—drives drug resistance among microbes and has made some of them virtually indestructible to modern medicine.
So, what exactly is antimicrobial resistance?
Antimicrobial resistance is the ability of bacteria/viruses/fungi/some parasites to survive the impact of antimicrobial agents (antibiotics, anti-fungal agents or antiviral agents) if they are constantly exposed to the same. All living beings have the ability to adapt. This is how species survive. So, if a microbe is constantly being exposed to an antimicrobial agent, it will eventually adapt and evolve to become more or fully resistant to antimicrobials that could previously treat it.
Why is antimicrobial resistance bad?
If a microbial species gets resistant to the antimicrobial agent, it makes the standard antimicrobial treatment ineffective. This results in non-treatment of the communicable disease caused by the microbial agent. It is important to note that the drug-resistant microbe reproduces and multiplies to form more drug-resistant microbes. The resistant bacteria can be transferred to humans through the food chain or direct contact. This can reduce the effectiveness of antimicrobials in treating diseases.
The infection spreads and it gets difficult to control it as the drug-resistant microbe spreads from one individual to another. As per Centers for Disease Control and Prevention (CDC), AMR accounts for 23,000 deaths per year in the United States.
Among the microbes that are now resistant to antimicrobial agents are some bacterial strains of salmonella and staphylococcus (both associated with food-borne illnesses and other infectious diseases).
What causes antimicrobial resistance?
Although antimicrobial resistance occurs in nature on its own, careless use and overuse of antimicrobial agents can accelerate the process. Antimicrobial resistance can be associated with factors such as over-prescription of antimicrobial agents such as antibiotics, consumption of antibiotics when one is suffering from viral infections such as common cold and flu, patients not sticking to the prescribed antimicrobial drug course, overuse of antimicrobial agents in animal agriculture, poor hygiene and sanitation practices that lead to frequent infections that in turn need antimicrobial drugs, poor infection control in healthcare settings which lead to spread of drug-resistant microbes, absence of new discoveries of antimicrobial drugs, and so on.
Suppose an antimicrobial agent is given to an animal over a long period of time. Let’s see what may happen as a result–
As this animal is exposed to a microbial regularly for a long period of time, the antimicrobials may not work when the animal catches an infection that is difficult to cure. Worse, the infection can spread to other animals.
Prolonged consumption of food products derived from such animals (egg, meat, dairy, etc.) by human beings can lead to development of antimicrobial resistance in the latter as well. When a human being catches an infection, the regular antimicrobial treatment course or dosage may not be effective enough.
Biopreservation and how it can help
Biopreservation refers to the technique of extending the shelf life of food by using natural or controlled microorganisms or their antimicrobial compounds or fermentation products. The fermentation products as well as beneficial bacteria are generally selected in this process to control spoilage and render pathogen inactive. Microbes that are harmless to humans, compete with spoilage and pathogenic bacteria, generate good odour, contribute in production of nice flavour, produce acids, antimicrobial substances and have fermentation capacity are used rather than those that have only fermentation property.
Certain lactic acid bacteria (LAB), with antimicrobial properties commonly associated with foods, are being used to increase the safety and/or prolong the shelf life of foods. Microbes thrive on nutrients to grow and multiply, and the presence of other microbes will necessarily limit the amount of nutrients available overall and thereby slow down the process of spoilage.
Related
Decoding Cyber Coverage in India: Your Ultimate Guide
In today's technology-driven landscape where digitalization is ubiquitous, companies confront an escalating threat landscape in the form of...
Navigating Insurance Options: Comprehensive Coverage for Diabetics in India
As the prevalence of diabetes continues to rise steadily in India, individuals grappling with this chronic condition encounter myriad challenges,...
Understanding International Travel Insurance
International travel insurance serves as a financial product crafted to shield travellers from unforeseen events and expenses while journeying...


